When you think of the fourth trimester, you picture endless newborn snugs. But for our warrior mama Gen, postpartum psychosis shook up her beautiful beginnings.
By Mama Disrupt®
The newborn bubble should be a blissful time of bonding and falling in love with your baby – but postpartum psychosis blindsided new mum Genevieve. Luckily, her partner Lizz spotted the signs and was able to help Gen get the support she needed. Here, they share their story.
“I THOUGHT THAT OUR CHILDREN, INCLUDING OUR NEWBORN ARLO, WERE ROBOTS.”
A good pregnancy
Genevieve and Lizz already had one child between them, with Lizz being the birthing parent. When they were ready for baby number two, Genevieve carried baby Arlo. “My pregnancy was relatively smooth,” she says. “Other than feeling sick at the thought of my usual daily coffee, I really didn’t have any morning sickness or experience any health concerns. I had planned to finish up work around one month before giving birth, but this did not go to plan.”
“The night before my last day of work, my waters broke. My partner and I were very much in shock (and excited) as we quickly tried to pack a hospital bag. She gave me a pre ‘push present’ before we left for the hospital – the book F**k, Now There Are Two Of You.”
Lizz was “nervous for Gen,” she says, “because I had been through a birth before as the birthing parent. (But) this was her first experience going through childbirth. I was concerned because I knew the level of pain she was going to go through. I didn’t want the process to go on for too long. My purpose was to be her support person. I did this in the best way I knew how – by making her laugh, encouraging her, and listening to her needs.”
The birth went smoothly, and Gen and Lizz welcomed their son Arlo into the world. But they had no idea what was to come.
“I didn’t realise that my role as a support person was going to extend for a considerable period after the birth,” Lizz recalls. She was not expecting to be thrust into the role of “primary sole carer for Arlo and an advocate for Gen.”

Back to hospital
Soon after the birth, Gen says, “I began to struggle with breastfeeding. Four days after giving birth I was discharged from hospital, but re-presented to ED that night with mastitis. Doctors would later find out that the mastitis was caused by a Strep B infection in my breastmilk. Following 48 hours of IV antibiotics, I was discharged on oral antibiotics. But two days later, the infection took over my body. I presented to the ED again. This time I was experiencing sepsis, a life-threatening response to the infection that can lead to death.”
Luckily, Lizz noticed the change in Gen – and it wasn’t just the infection. “I noticed a change in Gen’s behaviours and interactions with us,” she says. “She began to worry, and become fixated on situations within the environment and with people around us. I knew at the time that Gen was experiencing mastitis and I originally started to think that maybe she had signs of sepsis and delirium. The truth was that she was heading into a psychotic state of mind. I have to be honest, much of that time is a complete blur, raging adrenaline on my behalf – I was in fight or flight mode.”
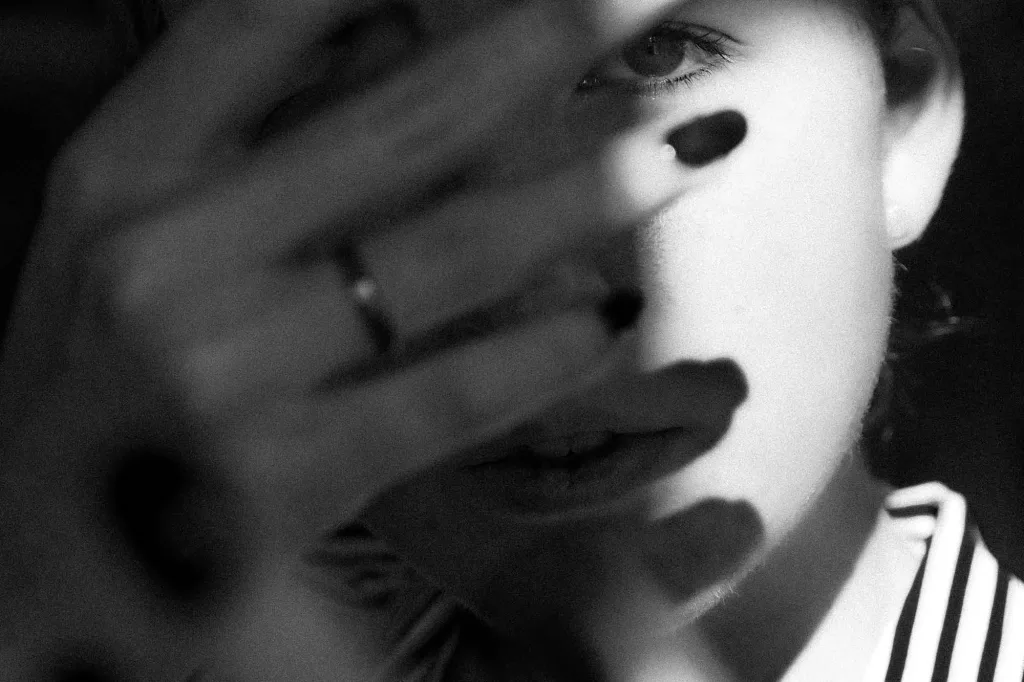
The beginnings of psychosis
Gen remembers suffering from “paranoia and delusions. I thought that the authorities were monitoring me for COVID-19, that I had been wired up by scientists who were controlling my body. And I thought that our children, including our newborn Arlo, were robots.”
“I spent two weeks in hospital being treated for the infection, during which time my partner noticed changes in my mental state. She advocated for a review by a psychiatrist, which led to many assessments and tests. Eventually I was diagnosed with postpartum psychosis.”

Getting help
“Once I was cleared from the infection,” Gen recalls, “I was transferred to an acute mental health ward where I continued my treatment for another two weeks. This whole time, I was not able to have my baby with me. So my partner was thrown into a sole parent role for our two kids, including Arlo, and a carer role for myself.
“Despite being a mental health nurse,” Lizz says, “and having seen some of the signs and symptoms of postnatal psychosis, it’s a whole other thing when your loved one requires containment, treatment and management under a psychiatric team. The role of ‘carer’ to my partner didn’t ever really enter my mind as a possibility.”
“(After my birth) I was the one who really struggled with postnatal depression and anxiety. Gen on the other had always been my rock during our original welcome to parenthood. She’s reliable, consistent, dependable, and accepting of all the quirkiness I’ve dished up over the years. But nothing prepared me for comments like, ‘do you think Arlo is real?’”
When she was ready, Gen says she was transferred to “a private mother and baby unit, to continue treatment and to re-build my bond with my baby. Following a couple of weeks in this unit, I felt confident enough to be discharged home and to start living my life with my family.”
“That was, until about one week later, when we were forced into our first COVID-related lockdown.”

Lockdown spiralling
“Arlo was born in early 2020,” Gen says, “just before COVID-19 was declared a pandemic. There were so many unknowns in 2020. Having a newborn at this time was extremely challenging. Community parent and baby groups were cancelled, healthcare was hard to access, and our support network shrank.”
Lizz had to go back to work full time, after having had the first seven weeks off to care for the kids. “This left me at home in lockdown,” Gen says, “and not allowed to invite family or friends over to meet our baby. I was isolated, without the usual support that loved ones can offer when you have a newborn. It was challenging, to say the least.”
“While the severe infection, sepsis, lack of sleep and hormonal changes led me into a delirium and eventual psychosis, I have no doubt that these external factors also contributed to my mental health issues following the birth of Arlo.”
As a result, she experienced a rebound depression in the six months following discharge. “But I continued to focus on recovery. With support from a community mental health team, and unwavering support and love from my partner and family, I was able to get through it.”

The silver lining
The couple describe the first year of Arlo’s life as “full of ups and downs.” But, they agree that the experience of postpartum psychosis ultimately brought them closer, both as a couple and as a family. “It’s common to hear that when someone experiences a health crisis, their perspective on life changes, and that’s how I feel,” Gen says. “We don’t take one another for granted. We reflect often on how lucky we are to have two beautiful, caring, thriving, and healthy boys. And we communicate openly and honestly with one another about how we are travelling and how we can create healthy boundaries, both as individuals and as a family.”

Mental health is #1
“We try to prioritise our mental health. This way we can be better partners to one another, and better parents for our kids.”
Navigating the maternal health system as a same-sex couple
“We had a wonderful experience with all our specialists, midwives and nursing staff. We believe we received the same level of care as cisgender heterosexual couples. However, there are always improvements that could be made across the health system to be more inclusive.
We’d like to see forms seeking people’s personal information ask for parent pronouns. We should replace mother/father language with parent/parent language. Health care professionals can be open and deliberate with their language, making no assumptions about family structure. For example, ask patients if they have a partner, rather than asking if they have a husband. Any resources to support soon-to-be or new parents can also shift their language, to be more inclusive of diverse families.”
For support with perinatal depression and anxiety, contact The Gidget Foundation.
Sign up to our newsletter for weekly mama goodness delivered straight to your inbox, like the VIP that you are.






